Alcoholic Hepatitis
Chronic alcohol abuse can lead to a number of serious illnesses. Among the more common is alcoholic hepatitis.
Although this illness mainly affects heavy drinkers, there are cases of moderate drinkers developing alcoholic hepatitis as well. If you drink regularly, it’s important to be aware of this condition, and how it can be treated or prevented.
What Is Alcoholic Hepatitis?
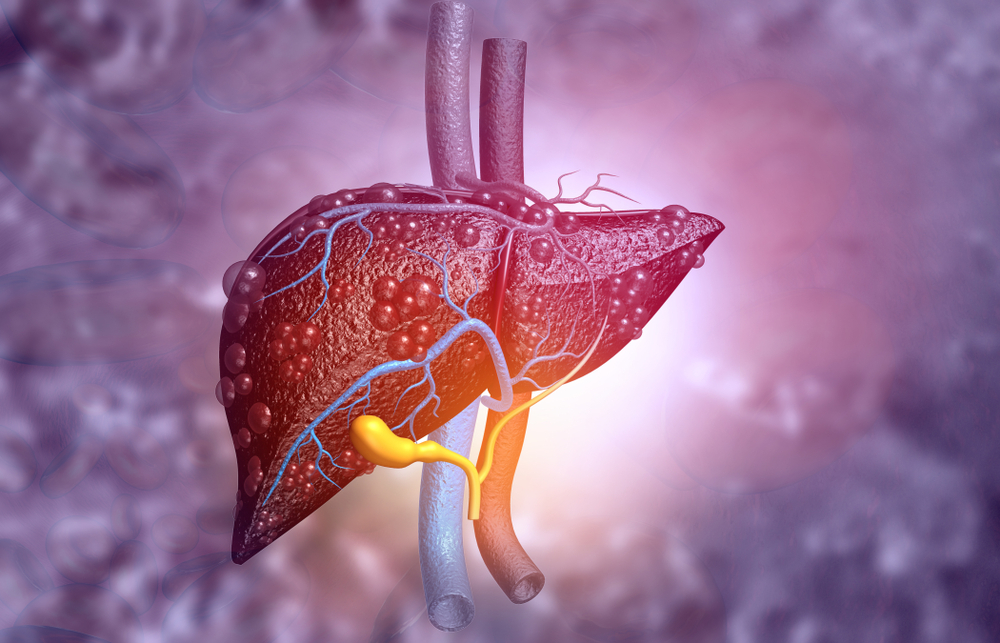
Alcoholic hepatitis is an inflammation of the liver caused by excessive alcohol consumption. According to the American Liver Foundation, alcoholic hepatitis occurs in up to 35 percent of heavy drinkers.
The condition varies in severity. Milder cases may develop slowly, and are often reversible if they are caught in time. Severe cases may develop quickly, and lead to life-threatening complications.
How Does Alcoholic Hepatitis Develop?
When you drink alcohol, your liver is responsible for breaking it down and removing it from your system. If you drink more than your liver can effectively process, it can place that organ under a lot of stress. If you do this chronically, it can eventually cause inflammation, the death of liver cells, and damage to your liver’s tissue.
Within the spectrum of alcohol-related liver disease (ARLD), alcoholic hepatitis is more serious than fatty liver, but not as severe as cirrhosis. However, it can still be life-threatening. Although this disease generally develops slowly over time, the acute form of alcoholic hepatitis can develop suddenly, rapidly leading to liver failure and even death.
Unlike viral forms of hepatitis (such as hepatitis B or hepatitis C), alcoholic hepatitis is not contagious. It is caused by alcohol use, not by a transmittable infection.
Who Is at Risk for Developing Alcoholic Hepatitis?
Alcoholic hepatitis is generally caused by excessive alcohol intake over an extended period of time.
How much is too much? The minimum threshold for high risk is approximately 40 grams of alcohol per day for a woman, and 50-60 grams per day for men. This is about 3-4 standard drinks per day. As for how long it takes, according to The World Journal of Hepatology people with alcoholic hepatitis have often drank at least 80 grams per day (more than 5 standard drinks) for over 5 years.
That said, things vary quite a bit from person to person. Periods of heavy alcohol use before developing alcoholic hepatitis can range from 3 months to 36 years. Even moderate drinkers occasionally develop alcoholic hepatitis, as do inconsistent binge drinkers.
Other factors include gender, genetic background, overall physical health, and even when you drink. If you tend to consume alcohol with food, you may have lower risk of alcoholic hepatitis. Obesity, on the other hand, can increase your risk. Women and African Americans seem to have a higher risk as well.
As far as age is concerned, alcoholic hepatitis is most common in people 40-60 years old. However, it has occurred in patients from 20-80 years of age.
Alcoholic Hepatitis Symptoms
Jaundice is among the most common signs of liver disease. If you notice your skin or the whites of your eyes becoming yellow, have a doctor check your liver. Other symptoms of alcoholic hepatitis include:
- Nausea and vomiting
- Abdominal tenderness
- Low grade fever (may also be a sign of infection)
- Weakness and fatigue
- Loss of appetite
- Weight loss
- Dark urine
- Dry mouth
- Easy bruising or bleeding
These symptoms may not appear right away, especially in milder cases.
If any combination of these occur over time, and you are drinking heavily and regularly, it is important to have yourself checked. Alcoholic hepatitis is a progressive disease, and can get worse the longer it goes untreated. Your doctor may perform a liver function test or liver biopsy for diagnosis, and ask about your history of alcohol use.
In addition to the possibility of liver failure, patients with alcoholic hepatitis may suffer from kidney disease, ascites (a buildup of fluid in the abdomen), high blood pressure, spider angiomas, hepatomegaly (enlarged liver), and even brain damage from toxins not removed by the liver.
Is Alcoholic Hepatitis Reversible?
In many cases, alcoholic hepatitis is reversible, especially if you catch it in the early stages. In later stages some or all of the damage to your liver may be permanent, and you may need a liver transplant. To prevent this worst-case scenario, your doctor may prescribe medication and/or nutritional support to help your liver repair itself. Dietary changes can also make a difference.
In most cases, you will also need to quit drinking alcohol completely. Because drinking both causes and aggravates alcoholic hepatitis, removing it is crucial to reversing this disease. No matter what stage you’re at, quitting alcohol is shown to improve recovery rates.
How Long Does It Take For Alcoholic Hepatitis To Resolve?
The length of time it takes to recover depends on how severe the case of alcoholic hepatitis is, and how early treatment begins. Within two years many patients show significant improvement, and appear to have normal liver function. For those with mild cases, recovery time can be quicker.
However, these improvements are dependent on patients continuing to abstain from alcohol, and some complications can remain for the long term. If you’ve recovered, you should continue to have yourself checked regularly for liver cancer. And if you’ve developed any cirrhosis of the liver from hepatitis, that damage will be permanent.
Can You Get Hepatitis B or C From Drinking Alcohol?
Although all forms of hepatitis involve inflammation of the liver, hepatitis B and C are specifically caused by viruses, and not by drinking alcohol. The main risk factors for developing either hepatitis B or C involve exposure to blood, semen, or other infected body fluids. Alcoholic hepatitis has many of the same long-term consequences, but it is not the same illness, and it is not contagious.
That said, there is some evidence that heavy drinking makes you more susceptible to contracting hepatitis C if you are exposed to the virus.
Can You Drink Alcohol When You Have Hepatitis B or C?
Alcohol is believed to weaken the body’s ability to fight off the hepatitis C virus. The relationship between hepatitis B and alcohol is less well understood, but appears to be similar. With hepatitis B, moderate drinking may be less risky. In both cases, however, it’s best to avoid heavy drinking at all costs.
If you have hepatitis B or C, check with your doctor about what amount of alcohol, if any, is safe. But your safest bet is to avoid drinking altogether.
Alcoholic Hepatitis vs. Cirrhosis
Cirrhosis is a permanent scarring of the liver. It is not the same condition as hepatitis, but it often develops as a result of it.
While liver damage from hepatitis is sometimes reversible, cirrhosis is not. And the more scar tissue you have in your liver, the harder it becomes for this vital organ to function. This can have many serious consequences for your overall health, and can eventually cause liver failure, which can be fatal. While some milder cases of cirrhosis are manageable, the only treatment for advanced cirrhosis is a liver transplant.
Unfortunately, cirrhosis is on the rise, making it more important than ever to raise awareness of this condition. And since alcoholic hepatitis can lead to cirrhosis, the sooner you catch liver damage—and reduce your alcohol consumption—the better.
Read More: Early Signs of Liver Damage From Drinking
Help For Reducing Your Drinking
If you’re struggling to cut back on your own, there are new solutions—including online programs like Ria Health. Our doctors can customize treatment to your unique needs, and even prescribe anti-craving medication that is safe for your liver. Best of all, you don’t need to identify as an alcoholic to join.
Find out how you can quit or cut back from the comfort of home, today.

Will insurance cover treatment? Verify Coverage
Have Questions? Call (800) 504-5360



