Hepatitis Can’t Wait: A Global Initiative
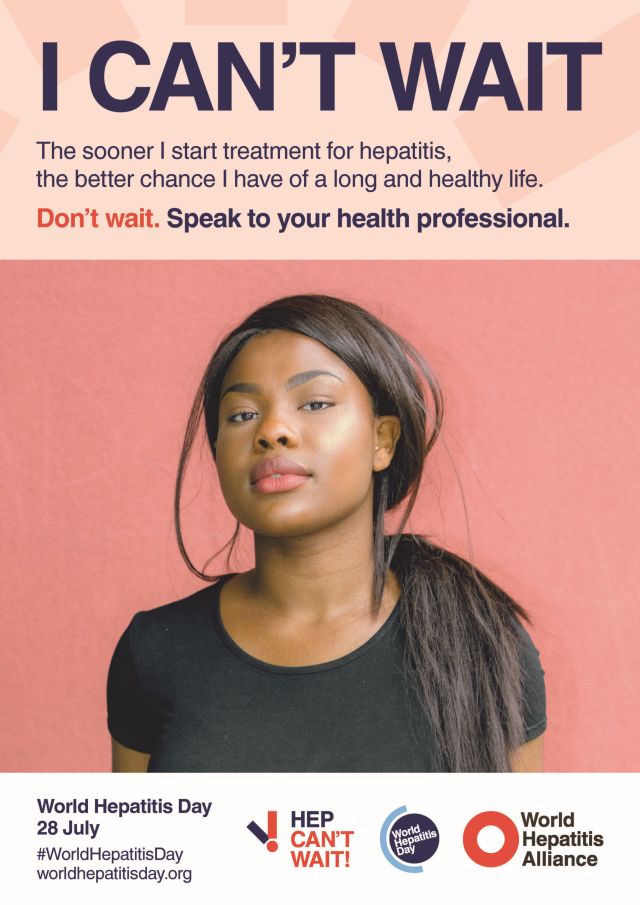
On Thursday, June 28, the World Hepatitis Alliance (WHA) marks World Hepatitis Day. This year’s campaign theme is “I Can’t Wait,” and reflects the urgency of getting tested for the disease. Some people are unaware that they may have been exposed to hepatitis and shouldn’t wait to get tested. The WHA estimates that 9 out of 10 people who have it are undiagnosed.
“I Can’t Wait” also refers to policy makers, who can make changes to end stigma and discrimination. Dealing with the disease avoids more serious conditions that can result later.
So what is hepatitis, and how is it transmitted? And what can help with symptoms? Answers come from some of the country’s most distinguished medical and health organizations.
What Is Viral Hepatitis?

Hepatitis can occur when the liver becomes inflamed. Exposure from someone else who has it, often by bodily fluids, is a common cause of viral hepatitis. Sometimes this exposure is through contaminated food or water, or in the case of hepatitis C, through sharing needles, e.g., for injecting heroin and other substances. Though hepatitis has five versions—designated by the letters A through E—the most common are A, B, and C, each caused by a different virus.
Symptoms can include jaundice (yellow skin and eyes), fatigue, lack of appetite, and other gastrointestinal issues. Recovering usually takes time, often weeks or even months. Most doctors recommend a regimen of nutritious food, lots of fluids, and plenty of rest. But appropriate vaccines can also prevent versions A and B.
What Is Alcoholic Hepatitis?
On the other hand, excessive alcohol use can also inflame the liver, and cause alcoholic hepatitis. Heavy drinking, especially over time, can overwhelm the liver, which is then unable to properly process alcohol. During the pandemic, some communities have seen a marked increase in this form of hepatitis, as well as other liver diseases.
If left unaddressed, alcoholic hepatitis can result in cirrhosis, liver failure, and death. The best way to prevent this is to stop drinking.
The WHA campaign focuses on viral hepatitis, rather than the alcohol-induced version. But one vital organ links the two conditions—the liver. Since this organ is the body’s primary means of getting rid of toxins, its role is critical.
As a side note, it’s true: viruses do not cause hepatitis that results from too much alcohol. But as the Cleveland Clinic notes, “Chronic heavy drinking can be ‘viral’ in the social sense. When friends or family binge drink together, they reinforce in each other the behavior that can lead to alcohol-induced hepatitis.”
Treatment for Hepatitis
Doctors recommend diet, plenty of fluids, and a lot of rest to treat viral hepatitis. It is not uncommon for full recovery to take weeks, sometimes months.
For alcohol-related hepatitis, the best treatment is to stop drinking—immediately. While we advocate for moderate drinking for many people if they choose, for someone diagnosed with hepatitis, the best solution is to not drink at all.
At Ria Health, many of our members want to simply cut back on alcohol—to be able to enjoy a beer or a glass of wine with friends now and then. Other members choose to stop drinking completely; for them, even a small bit of alcohol is not only physically unhealthy, but can trigger old drinking patterns and behavior.
Hepatitis can quickly turn into a serious issue, leading to liver damage that can be difficult to reverse. If you or someone you love is having problems with alcohol, now there are more options than ever. Call or write to us today, and let us show you a convenient, effective, and affordable way to change your relationship with alcohol—for good.
Will insurance cover treatment? Verify Coverage
Have Questions? Call (800) 504-5360



